No One Can Find the Rewind Button Now, So Cradle Your Head in Your Hands...
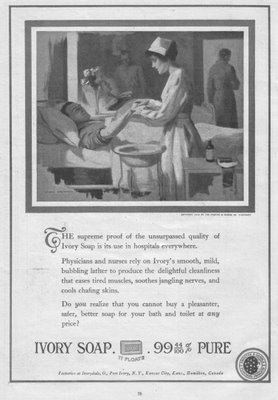 What a freakin' wimpy bedbath!
What a freakin' wimpy bedbath!
Gee, we don't want to overexpose our patient, now do we?
She looks like she's giving him a manicure!
And I guess we don't need privacy because nothing is showing! What's she going to do when she gets past (shock!) the elbow?
Were axilla off limits back then?
Well, at least according to the ad, the patient will experience a "delightful cleanliness"....of his distal phalanges.
I believe in truth in advertising so I've never understood how Ivory gets away with saying it is 99 and 44/100% pure.
What's in the other 56/100%
Ebola?
hhhhhhhhhhhhhhhhhh
It was just supposed to be a quick four-hour shift.
I have a co-worker who has trouble with twelve hours shifts, as I do. She was scheduled for one tonight and I offered to do the first four in her place.
The unit was down to two patients, the break table full of Easter goodies and a kick-back attitude was to be had by all.
All the prerequisites for a Code 3 ringdown.
It came.
Cardiopulmonary arrest. Elderly. Found by spouse. Resuscitated en route. Still unresponsive but with a blood pressure, a pulse and (God bless all medics, every one) intubated with an IV. Technically was a DNR but papers were with the patient's doctor and not at home.
Lots and lots of activity. Many tubes placed where tubes usually go (foley, ng) and then a few new holes placed for those tubes that don't have a regular hole to fit it (central line). Many cooks in the broth. Much help to be had.
It did not look good.
The family decided that the ventilator would be removed and oxygen supplied through the ET tube.
Slowly but surely, the other nurses went back to their assignments and somehow I was the one who would be staying with the family until the patient expired, explaining what was happening.
I could insert a joke here, about the Energizer Bunny or the patient being like a Timex that takes a lickin' and keeps on tickin'.
But they really don't fit in this narrative.
My patient did not expire for over one hour.
During that hour I heard stories of what it was like to be married to, and now losing, a spouse of 70 years. We laughed over reminiscences the family shared. How one of the grandkids was the spitting image of the patient as a young person.
How one of the last things shared at Easter dinner just a few hours before was the patient saying what a good life they had had with their spouse. How happy they were.
How they had gotten the okay to travel abroad in four weeks. In their nineties.
I sat on one side of the patient holding their hand and the family sat on the other, stroking and holding the other arm. I offered them my place, but it seemed they found strength in leaning on each other.
And then, slowly, the resuscitation medications began to wear off and heart began to slow. Gradually, gradually until I documented asystole and turned off the monitor and oxygen.
Pretty technical.
Except that tonight there is a person who will be facing life on their own for the first time in seventy years.
Except that tonight there are adult children who are dealing with the loss of their parent. Grandchildren who will wish they had more time to know their grandparent.
Except for the fact that every time we lose a person who has lived as long as ninety years, we lose a treasure, a link to the past; a wealth of memories and experiences that will soon be relegated to textbooks.
Except for the fact that in ER, patients die quickly before you usually have a chance to get to know them or their families.
I haven't sat vigil with a patient and their family like that for many years. The opportunity to do so does not present itself often in the ER environment.
I have a co-worker who has trouble with twelve hours shifts, as I do. She was scheduled for one tonight and I offered to do the first four in her place.
The unit was down to two patients, the break table full of Easter goodies and a kick-back attitude was to be had by all.
All the prerequisites for a Code 3 ringdown.
It came.
Cardiopulmonary arrest. Elderly. Found by spouse. Resuscitated en route. Still unresponsive but with a blood pressure, a pulse and (God bless all medics, every one) intubated with an IV. Technically was a DNR but papers were with the patient's doctor and not at home.
Lots and lots of activity. Many tubes placed where tubes usually go (foley, ng) and then a few new holes placed for those tubes that don't have a regular hole to fit it (central line). Many cooks in the broth. Much help to be had.
It did not look good.
The family decided that the ventilator would be removed and oxygen supplied through the ET tube.
Slowly but surely, the other nurses went back to their assignments and somehow I was the one who would be staying with the family until the patient expired, explaining what was happening.
I could insert a joke here, about the Energizer Bunny or the patient being like a Timex that takes a lickin' and keeps on tickin'.
But they really don't fit in this narrative.
My patient did not expire for over one hour.
During that hour I heard stories of what it was like to be married to, and now losing, a spouse of 70 years. We laughed over reminiscences the family shared. How one of the grandkids was the spitting image of the patient as a young person.
How one of the last things shared at Easter dinner just a few hours before was the patient saying what a good life they had had with their spouse. How happy they were.
How they had gotten the okay to travel abroad in four weeks. In their nineties.
I sat on one side of the patient holding their hand and the family sat on the other, stroking and holding the other arm. I offered them my place, but it seemed they found strength in leaning on each other.
And then, slowly, the resuscitation medications began to wear off and heart began to slow. Gradually, gradually until I documented asystole and turned off the monitor and oxygen.
Pretty technical.
Except that tonight there is a person who will be facing life on their own for the first time in seventy years.
Except that tonight there are adult children who are dealing with the loss of their parent. Grandchildren who will wish they had more time to know their grandparent.
Except for the fact that every time we lose a person who has lived as long as ninety years, we lose a treasure, a link to the past; a wealth of memories and experiences that will soon be relegated to textbooks.
Except for the fact that in ER, patients die quickly before you usually have a chance to get to know them or their families.
I haven't sat vigil with a patient and their family like that for many years. The opportunity to do so does not present itself often in the ER environment.
ddd
The family left.
I went into the bathroom and cried for two minutes....
... and then came out and made the requisite calls to the coroner and the donor network, finished my charting, posted my strips, circled my charges and swiped out for the night.
ddd
I went into the bathroom and cried for two minutes....
... and then came out and made the requisite calls to the coroner and the donor network, finished my charting, posted my strips, circled my charges and swiped out for the night.
ddd
Another death.
Another holiday.
Something tells me I will have another "yearly visitor" around Easter next year.
And that gives me comfort.
In the meantime, I'll take the advice in the song written by Anna Nalick from which I took the title of this post and cradle my head in my hands.
And breathe.
Just breathe.
Another holiday.
Something tells me I will have another "yearly visitor" around Easter next year.
And that gives me comfort.
In the meantime, I'll take the advice in the song written by Anna Nalick from which I took the title of this post and cradle my head in my hands.
And breathe.
Just breathe.











7 Comments:
Kim, thank you. That was beautiful, and made me cry.
It was this month, last year, that we lost my 90 year old father-in-law ... my sweet, dear, partner in crime. Your post just made it all real to me again.
A lot has happened in a year.
Keep posting Kim ... please keep posting.
Lucky patient to have you at his side while he transitioned from this life to the next. Lucky family to have you as well. Thank you for sharing and for making such a hard time just a bit easier for this family.
She DOES look like she's giving a manicure!
Do you realize how difficult that was to read, and all because you kept using "they" in place of the correct pronoun "he" or "she"? Sometimes you used "their" to mean "his" and sometimes you used "their" to actually mean "their" (as in "belonging to the couple"). Why would you do that? It's against the rules of English and makes your writing inscrutable.
Anonymous: thanks for pointing that out. It read OK to me because I knew what I meant but I can see where confusion would reign.
It was an attempt to keep patient identity as "inscrutable" as possible.
When there is an episode or incident that is relatively recent, I try not to assign either sex to the patient.
But, knowing that it makes the post hard to decipher/read, I'll try to find a more appropriate way to disguise an identity.
Sincerely, thank you for the feedback.
Blogging has been terrible for my English. I read that entire post, and did not notice the "they's" until I read that comment. I too, try to keep everything I say gender-neutral, and now read and write that way without any problem...
A great post... As a fairly new nurse, I've only had to deal with the death of a patient in my care once, but as a CNA I dealt with it a lot. I think its great that you were able to devote that time to the family in an ER environment. I know it was appreciated!
As difficult as vigil may be, it is, as you recognized, also uniquely rewarding. You supported the patient, and the family, in a difficult but necessary transition. I am sure the family was blessed by your presence, and your ability to accept death as both a part of life and a chance to rejoice and recollect the past. You are one heck of a nurse!
Post a Comment
<< Home